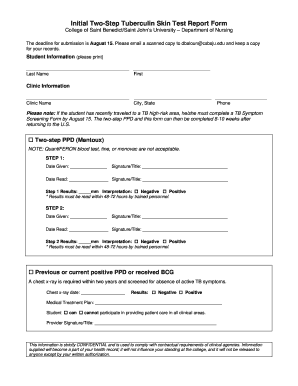
MSU UPHYS TB Skin Test Reporting free printable template
Show details
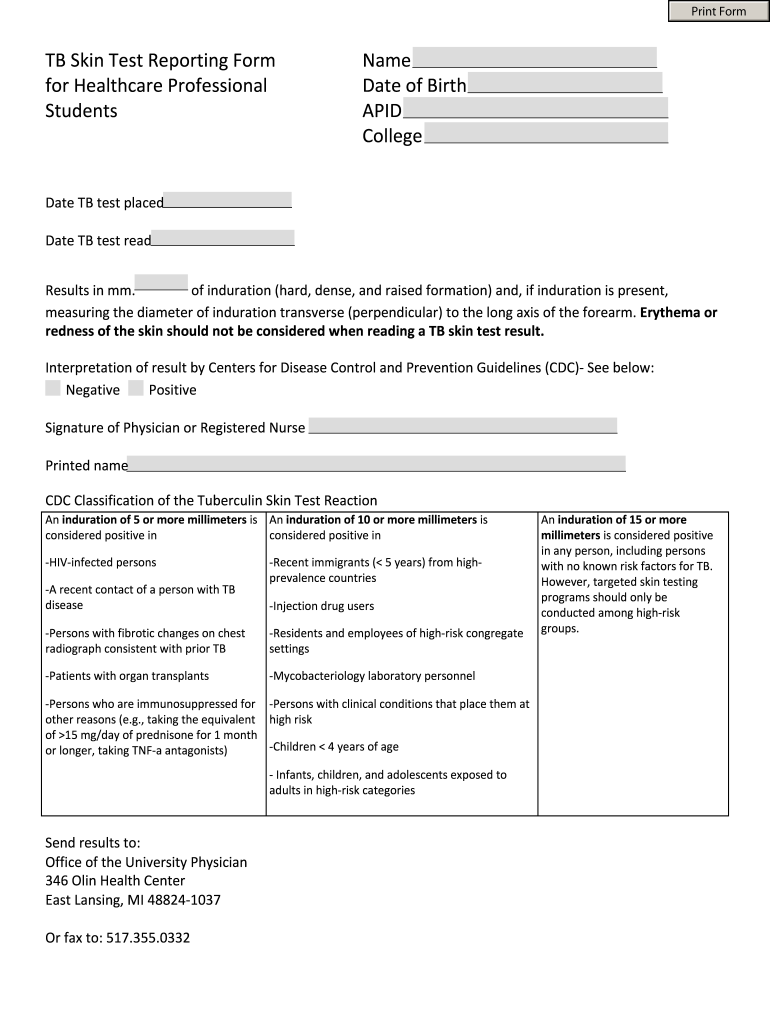
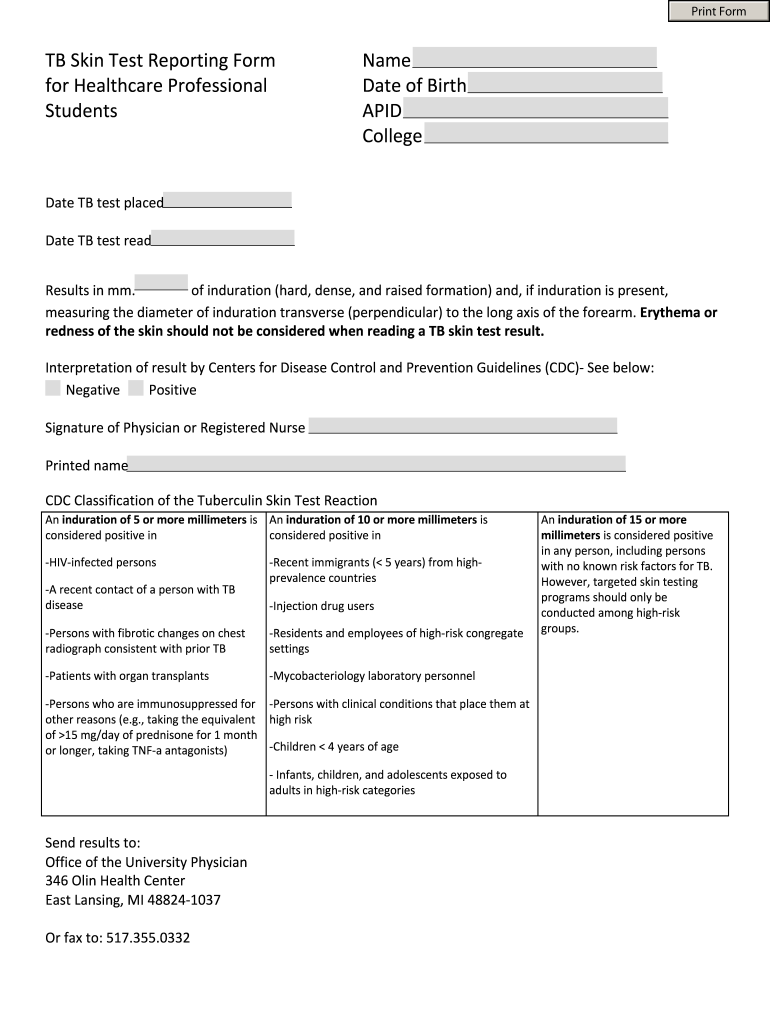
Print Form TB Skin Test Reporting Form for Healthcare Professional Students Name Date of Birth ACID College Date TB test placed Date TB test read Results in mm. of induration (hard, dense, and raised
pdfFiller is not affiliated with any government organization
Get, Create, Make and Sign printable blank tb test form

Edit your tb skin test form pdf form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.

Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.

Share your form instantly
Email, fax, or share your nurse choice tb test form form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit printable tb test form online
Follow the steps down below to take advantage of the professional PDF editor:
1
Set up an account. If you are a new user, click Start Free Trial and establish a profile.
2
Upload a document. Select Add New on your Dashboard and transfer a file into the system in one of the following ways: by uploading it from your device or importing from the cloud, web, or internal mail. Then, click Start editing.
3
Edit blank printable tb test form. Add and replace text, insert new objects, rearrange pages, add watermarks and page numbers, and more. Click Done when you are finished editing and go to the Documents tab to merge, split, lock or unlock the file.
4
Get your file. When you find your file in the docs list, click on its name and choose how you want to save it. To get the PDF, you can save it, send an email with it, or move it to the cloud.
pdfFiller makes working with documents easier than you could ever imagine. Create an account to find out for yourself how it works!
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out tb test form

How to fill out MSU UPHYS TB Skin Test Reporting Form
01
Obtain the MSU UPHYS TB Skin Test Reporting Form from the appropriate health department or website.
02
Fill out the patient's personal information including name, date of birth, and contact details.
03
Indicate the date the TB skin test was administered and the date it was read.
04
Record the results of the TB skin test, including the measurement in millimeters.
05
Provide details of the administering healthcare professional, including name and credentials.
06
Sign and date the form to certify the accuracy of the information provided.
07
Submit the completed form to the designated health department or school office.
Who needs MSU UPHYS TB Skin Test Reporting Form?
01
Individuals who are required to undergo TB testing for school entry or compliance with health regulations.
02
Healthcare workers who need to provide proof of TB testing for employment.
03
Individuals entering programs that require proof of TB testing, such as nursing or medical school.
Fill
tb skin test form
: Try Risk Free






People Also Ask about tuberculosis form pdf
Does tuberculosis need to be reported?
Any patients with confirmed or suspected active TB disease are required by law to be reported within 1 working day of identification to the TB Control Section. This includes any patient that has started empiric multi-drug therapy for active pulmonary/extra-pulmonary TB.
How do I report TB in Florida?
The Florida Department of Health is here to serve you. Contact us with any questions you may have regarding Tuberculosis at 850-245-4350.
How do I document my TB test results?
TST Documentation Requirements Name and signature of person administering test. Date and time test administered. Location of test (e.g., right forearm, left forearm, alternate site) Tuberculin manufacturer, lot number and expiration date.
Is tuberculosis a reportable disease in USA?
Active TB disease Both pulmonary and extrapulmonary forms of TB disease are reportable. To report a confirmed or suspected case of TB disease, call the TB Prevention and Control Program at 651-201-5414 or 1-877-676-5414, or fax 1-800-296-0993.
Why does TB have to be reported?
Reporting cases of suspected or confirmed tuberculosis is vital to protect public health as it allows the Health Department to intervene in order to interrupt disease transmission.
How to bill for TB skin test reading?
How do we bill for placing the skin test for tuberculosis? To bill for placing the purified protein derivative (PPD) skin test for tuberculosis, use CPT®code 86580. Use this code when the nurse or medical assistant places the test on the patient's skin.
Our user reviews speak for themselves
Read more or give pdfFiller a try to experience the benefits for yourself
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I modify printable tb skin test form without leaving Google Drive?
Using pdfFiller with Google Docs allows you to create, amend, and sign documents straight from your Google Drive. The add-on turns your tb results form into a dynamic fillable form that you can manage and eSign from anywhere.
How do I fill out printable tb skin test form pdf using my mobile device?
On your mobile device, use the pdfFiller mobile app to complete and sign tb test paper. Visit our website (https://edit-pdf-ios-android.pdffiller.com/) to discover more about our mobile applications, the features you'll have access to, and how to get started.
How do I complete tb test form printable on an Android device?
On Android, use the pdfFiller mobile app to finish your tb test sheet. Adding, editing, deleting text, signing, annotating, and more are all available with the app. All you need is a smartphone and internet.
What is MSU UPHYS TB Skin Test Reporting Form?
The MSU UPHYS TB Skin Test Reporting Form is a document used to record and report the results of tuberculosis (TB) skin tests conducted on individuals associated with Michigan State University.
Who is required to file MSU UPHYS TB Skin Test Reporting Form?
Individuals who perform TB skin tests, including healthcare professionals and students in health-related programs, are required to file the MSU UPHYS TB Skin Test Reporting Form.
How to fill out MSU UPHYS TB Skin Test Reporting Form?
To fill out the MSU UPHYS TB Skin Test Reporting Form, you need to provide the individual's personal information, test date, results of the skin test, and any other relevant medical information as specified on the form.
What is the purpose of MSU UPHYS TB Skin Test Reporting Form?
The purpose of the MSU UPHYS TB Skin Test Reporting Form is to ensure accurate documentation and reporting of TB skin test results, which aids in the monitoring and control of tuberculosis in the university community.
What information must be reported on MSU UPHYS TB Skin Test Reporting Form?
The information that must be reported on the MSU UPHYS TB Skin Test Reporting Form includes the individual's name, date of birth, test date, results (positive or negative), administration site, and the name of the person who administered the test.
Fill out your MSU UPHYS TB Skin Test Reporting online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.
Blank Tb Test Form is not the form you're looking for?Search for another form here.
Keywords relevant to tb form printable
Related to tb test template
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.